Tuesday Feb 24, 2026
Tuesday Feb 24, 2026
Wednesday, 13 August 2025 00:08 - - {{hitsCtrl.values.hits}}
When the virus remains in the liver for many years, gradual damage could take place
 |
| Asther Whitefield, Bangalore Hospital Hepato Pancreato Biliary and Multi Organ Transplantation Senior Consultant Dr. H.R.S. Girn |
By Fathima Riznaz Hafi
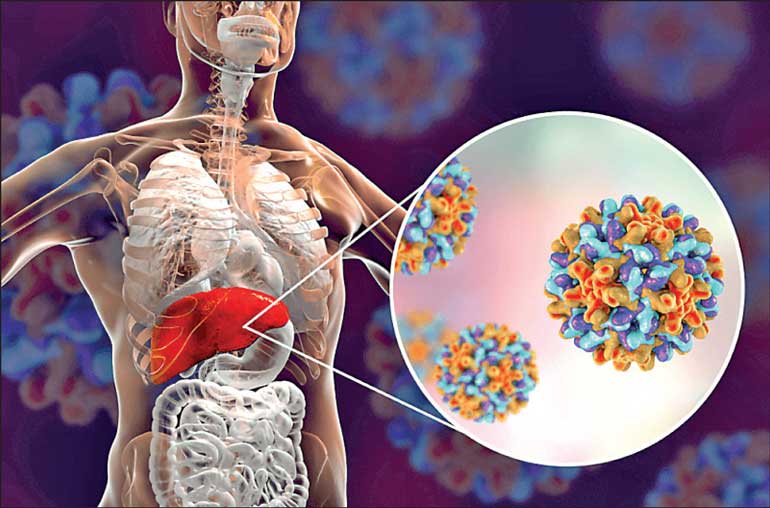
After a patient diagnosed with Hepatitis B has gone through the sickness phase, been treated and cured, the story doesn’t end there. The patient will feel better after recovery and life gets back to normal, but the virus remains in the liver. It stays there permanently (and silently), and over the long term, this could lead to cirrhosis or even liver cancer.
This uncanny fact was shared by Asther Whitefield, Bangalore Hospital Hepato Pancreato Biliary and Multi Organ Transplantation Senior Consultant Dr. H.R.S. Girn, at a recent press meet in Colombo, facilitated by A Mart Holdings, the hospital’s official representative in Sri Lanka. Dr. Girn carries expertise in advanced hepatobiliary surgeries and multi-organ transplantations, with international experience, practicing in UK and India.
Follow-up vital
“When the virus remains in the liver for many years, gradual damage could take place in that organ, eventually resulting in cirrhosis in some patients and possibly liver cancer in some. This can be prevented if follow-up tests are done consistently from the onset of the disease. This is vital. The patient needs to get himself tested every year, to monitor the liver and keep the replication of the Hep B virus under control to avoid progressive damage of the liver,” Dr. Girn says.
“For Hep B and C, a viral PCR has to be done at least once a year. From the onset of that disease, patients need to get screened regularly, forever,” he added.
“And in the eventuality that damage is detected, the patient will be treated but we can never eliminate the virus – ever!”
This happens only with the Hep B and C virus. Hep A, E, and the other viruses leave the liver completely; hence, once the patient is cured, he remains virus-free and healthy. With Hepatitis A and E there is no permanent damage. 2-4% of the patients will move to liver failure but otherwise for the other patients there is no lasting sickness.
“For Hepatitis B we have a vaccine, so it is preventable. For Hepatitis C we don’t have a vaccine. While people who get Hepatitis B or C should be followed up, this is not necessary for Hepatitis A and E. Hepatitis B and C are the problem – due to the virus remaining there permanently,” he explained.
Blood tests not sufficient
Dr. Girn says blood tests alone are not sufficient to detect liver problems. They need to be combined with scans for a clearer outcome. “We need biometric tools. Most people go for antibody tests but those tests are not enough because the liver regenerates. Think about this: How do I manage to take 60-70% of the healthy liver out? That is because the liver regrows. Imagine that modification – that capacity is enormous. So if I have a fatty liver, my liver tries to make more cells; I binge drink in the night and kill a lot of my liver cells, next, my cells are regenerating themselves.
 “So we may have undergone structural changes like cirrhosis because of years of abuse, but our blood test may be normal! Because our liver has a regeneration capacity. Hence, it’s important to combine the blood tests with visual products, or screening products – such as ultrasounds and fibroscans.”
“So we may have undergone structural changes like cirrhosis because of years of abuse, but our blood test may be normal! Because our liver has a regeneration capacity. Hence, it’s important to combine the blood tests with visual products, or screening products – such as ultrasounds and fibroscans.”
An ultrasound tells you about the shape or if there are any lesions in the liver. It tells you about the size of the bile ducts, and the size of your spleen, so it can co-relate that information with your blood results. A fibroscan is more specific – it will tell you how hard the liver is or what stage of fatty liver you are in.
Particularly when you are slightly older you should not rely on blood results too much; the results will be up and down a bit; it’s not a very big deal. Just having blood tests done is a big mistake. For younger patients, blood tests are sufficient, but more caution is needed for the older patients; hence, the combination of blood tests and scans are vital for this group, he said.
Regular screening is key
The doctor was asked, with the liver regrowing and regenerating, doesn’t it help in the case of the Hep B virus remaining in the liver and causing long-term damage? He replied, “No; if someone has diagnosed Hepatitis B and C, the recommendation world-over is they should get a minimum of one ultrasound scan a year. In 25% of patients with Hepatitis B, one out of every four will develop cirrhosis or liver cancer. We don’t know whether it will happen in 10 or 20 years. We don’t have the tools to assess that. So the answer is they should have a minimum of one ultrasound scan a year and six-monthly blood tests, including the virus titus (PCR test) after they’ve had hepatitis, to see if the numbers are there. Someone who has had Hepatitis B or C, even if they have been treated, should get a viral PCR test done at least once a year to see whether the levels are there.”
“But what happens is, most people go only for anti-body tests and those tests are not useful because once they get infected the antibody results stay positive for the rest of their lives; we need to know if there’s an actual virus roaming around in the liver. The patient should first get the scan at least once a month and if there are changes taking place in the liver, we can change the schedule to every six months, depending on the patient. The answer is to get the basic level of screening and get it done consistently,” he explained.
“Usually, it’s when a person has the Hepatitis virus and fatty liver together, that it turns into cirrhosis. They may be drinking frequently and develop fatty liver. So lifestyle can contribute to this.
“But that doesn’t mean that every patient who has fatty liver will end up with cirrhosis. There are many patients who have had fatty liver for years and never developed cirrhosis. Likewise, many patients who had Hepatitis B or C never developed cirrhosis. Right now we don’t have the tools to identify who is at risk or needs to be screened. The key is to get yourself scanned regularly to detect any danger signs early,” he advised.
Fatty liver completely reversible
 Dr. Girn went on to speak about the misconceptions surrounding fatty liver disease and cirrhosis. When a person is diagnosed with fatty liver, it is widely understood that he has met his doom. This is because fatty liver is feared as a deadly ailment with no cure. He says that is a misconception and that fatty liver, with the right medical intervention, is completely reversible.
Dr. Girn went on to speak about the misconceptions surrounding fatty liver disease and cirrhosis. When a person is diagnosed with fatty liver, it is widely understood that he has met his doom. This is because fatty liver is feared as a deadly ailment with no cure. He says that is a misconception and that fatty liver, with the right medical intervention, is completely reversible.
“Fatty liver doesn’t necessarily mean cirrhosis. Fatty liver is a biomarker of many things. Fatty liver is reversible. That’s good news. With state-of-the-art screening and subsequent treatment now available, there are higher chances of getting cured of liver diseases, even something as serious as fatty liver.” He added, however, that fatty liver is only reversible when the patient is in the ‘reversible’ stage. When the patient has delayed screening and sought help long after liver damage has taken place it would have reached an irreversible stage. He therefore stressed again that early detection through scans is vital.
He noted that prevention would be better and that would be by practising good health habits. If a person has unhealthy habits, the resulting disorders would exacerbate liver damage, increasing the risks of developing fatty liver. “If they are careless about drinking, it’s highly likely they are careless about their food as well,” the doctor noted. This compounds their risk of developing liver disease.
“About 50-60% of the patients who go for liver transplant have fatty liver involvement, in one way or other. They are people who are not drinking a lot. They are not eating healthy. If someone is careless in one extent they are also careless in other extents. So it is not always alcohol-related. Fatty liver can occur in non-alcoholics as well.
“Knowing that they drink frequently, and alcohol makes them more prone to fatty liver and other liver diseases, it is advisable that they take the responsibility of getting their liver screened regularly,” he stated.
“We have a biomarker now – to tell you whether you have the potential of generating this disease. When damage is detected, we can take steps to reverse it. Though liver transplantation is an option, the best step is to reverse it – you don’t need to start thinking about transplantation, you need to think of reversing.” The liver regrows, thus facilitating reversal. And with state-of-the art detection and treatment facilities now available, fatty liver disease should no longer mean the end of the road, he asserted.
Lifestyle – moderation in everything
The doctor noted that moderation in our daily practices plays a positive role in our wellbeing. “When it comes to lifestyle, moderation is important – moderation in everything – moderation in eating, moderation in your alcohol, and moderation in your work-life balance in terms of having time for a regular workout. Sure, a percentage of the problem is due to genetic disposition, but about 90% of these are lifestyle-induced. Generally, if you have moderation in your life you’ll be fine.”
 He went on to say, “We all need exercise; walking is not good enough; walking is not an exercise – we need to work on our back, and thighs and legs – we need to build the muscles – and prevent diseases like osteoporosis. Brisk walking is alright – provided you do a substantial bit and for a substantial time. It has to be a solid, brisk walk for about 45 minutes even if it’s on a treadmill and 7.5 kilometres walk-time and regularly, then I can call that an exercise. But when you say walking, many people just go around the lawn for 15 minutes and call it exercise. That’s not good enough.”
He went on to say, “We all need exercise; walking is not good enough; walking is not an exercise – we need to work on our back, and thighs and legs – we need to build the muscles – and prevent diseases like osteoporosis. Brisk walking is alright – provided you do a substantial bit and for a substantial time. It has to be a solid, brisk walk for about 45 minutes even if it’s on a treadmill and 7.5 kilometres walk-time and regularly, then I can call that an exercise. But when you say walking, many people just go around the lawn for 15 minutes and call it exercise. That’s not good enough.”
He also suggested taking up exercises like static cycling rather than just walking, and noted rowing, cycling, swimming are all very good exercises. We have to push ourselves as we get older. We may not do that when we are younger but later that will become a problem, the doctor cautioned. He recommended having a workout routine – focus on things that we can do.
Generally, taking care of ourselves is key. Screening along with a good lifestyle is the way to go about this. Get the necessary tests after the advised age. Get a dexascan every five years. It is good to have blood tests after we reach our 40s and go for at least yearly check-ups. We have to push ourselves as we get older, he advised.