Sunday Feb 22, 2026
Sunday Feb 22, 2026
Tuesday, 14 November 2023 00:20 - - {{hitsCtrl.values.hits}}

Dr. Chameera Bandara
In an interview with the Daily FT, Consultant Eye Surgeon and Oculoplastic Surgeon from the National Hospital of Sri Lanka, Dr. Chameera Bandara elaborates on the importance of keeping diabetes at bay to assure optimum eye health.
 By Randima Attygalle
By Randima Attygalle
It is well established that diabetes is not an isolated disease. It is a multi-system disease which is a major cause of blindness, kidney failure, heart attack, stroke and lower limb amputation. The prevalence of diabetes, as the WHO notes, has been rising more rapidly in low and middle-income countries than in high-income countries. Between 2000 and 2019, there was a 3% increase in diabetes mortality rates by age as the WHO data confirm.
Diabetes-induced eye problems are on the rise with more young people now diagnosed with diabetes. The increased life span of people too contributes to growing numbers, says National Hospital of Sri Lanka, Consultant Eye Surgeon and Oculoplastic Surgeon, Dr. Chameera Bandara. “Diabetes related eye issues could be broadly categorised as intraocular issues (problems within the eyeball) and others indirectly related to eye functioning such as problems in the surrounding tissues, nerves, muscles and the brain. Any complication in the eye ball directly affects the vision of a person. Other issues could range from droopiness of upper-lid to double vision,” explains Dr. Bandara.
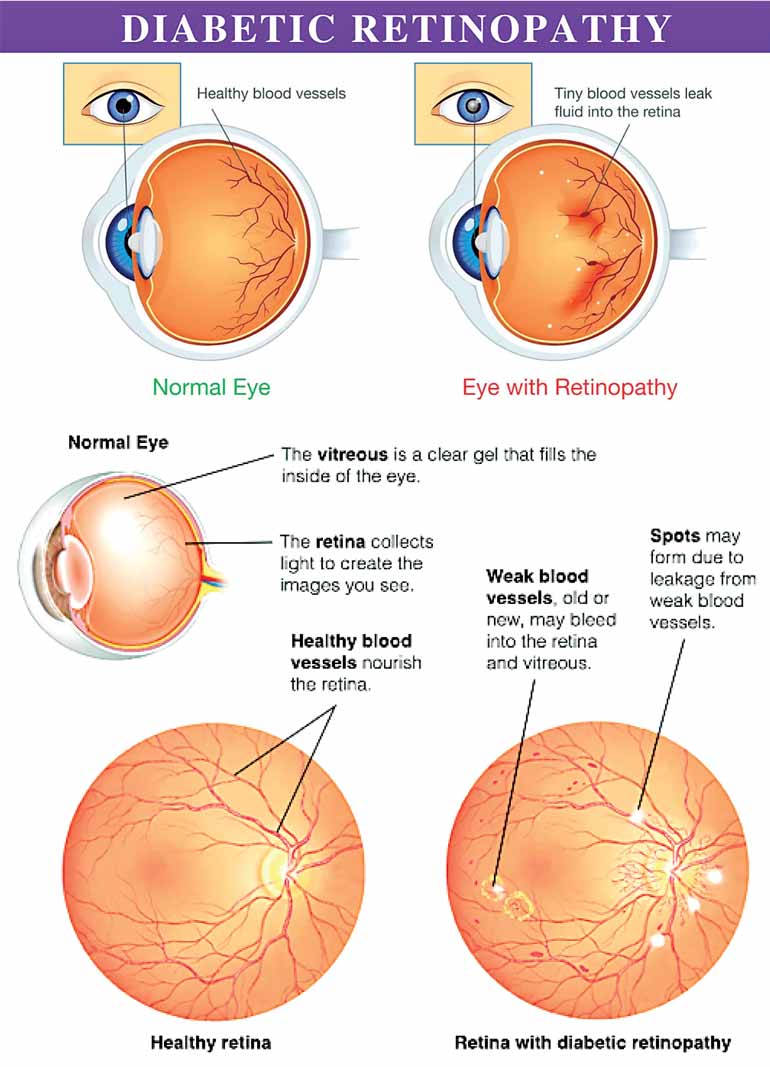
Diabetic retinopathy
The commonest intraocular complication that is diabetes-related is what is known as ‘diabetic retinopathy’. The WHO has estimated that diabetic retinopathy is responsible for 4.8% of the 37 million cases of blindness throughout the world. The risk of diabetic retinopathy increases with prolonged diabetes in a person. “Those with Type 1 diabetes or insulin-dependent diabetes which usually appears during childhood or adolescence are at a higher risk of developing diabetes retinopathy as they would have to live with diabetes longer than those with Type 2 diabetes, often found in those over 45 years. However, the condition could develop in those with Type 2 diabetes as well.” In addition to poorly controlled diabetes, other conditions such as hypertension, high cholesterol levels, anemia or kidney problems could increase the chances of diabetic retinopathy. “The longer you have diabetes and the less controlled your blood sugar is, the chances are more for you to develop this condition,” warns the Consultant.
Complications of diabetic retinopathy
 Diabetic retinopathy is of two stages: non-proliferative diabetic retinopathy (NPDR) and proliferative diabetic retinopathy (PDR).
Diabetic retinopathy is of two stages: non-proliferative diabetic retinopathy (NPDR) and proliferative diabetic retinopathy (PDR).
NPDR is the early stage of the disease when the walls of the blood vessels in the retina weaken. Tiny bulges protrude from the walls of the smaller vessels (micro-aneurysms), sometimes leaking fluid and blood into the retina. NPDR can progress from mild to severe as more blood vessels become affected. Sometimes tiny whitish particles called exudates can form in the retina from leaked cholesterol materials.
Sometimes retinal blood vessel damage leads to a buildup of fluid (edema) in the centre portion (macula) of the retina. When the macula swells, it is called ‘macular edema’. “This is the most common reason why people with diabetes lose their vision,” points out Dr. Bandara.
Moreover, with NPDR, blood vessels in the retina can close off. This condition is called ‘Retinal ischemia’. “In the  case of macular ischemia, blood cannot reach the macula and can affect a person’s vision.”
case of macular ischemia, blood cannot reach the macula and can affect a person’s vision.”
Diabetic retinopathy can progress to a more severe type, known as proliferative diabetic retinopathy (PDR). In PDR, damaged blood vessels close off, causing the growth of new, abnormal blood vessels in the retina. Complications of PDR are many:
Vitreous hemorrhage. The new blood vessels may bleed into the clear, jellylike substance that fills the centre of the eye, called the vitreous. If the amount of bleeding is small, one may see only a few dark spots (floaters). In more-severe cases, blood can fill the vitreous cavity and completely block the vision. “Vitreous hemorrhage per se doesn›t cause permanent vision loss unless the retina is damaged. The blood often clears from the eye within a few weeks or months and the vision would likely return to its previous state. Persistent or slowly resolving vitreous hemorrhage may be benefited by surgical clearance,” explains the Consultant.
Retinal detachment. The abnormal blood vessels associated with diabetic retinopathy stimulate the growth of scar-like tissue, which can detach the retina away from the back of the eye. This can cause spots floating in a person’s vision, flashes of light or severe vision loss.
Neovascular Glaucoma. New blood vessels can grow in the front part of your eye (iris) and interfere with the normal flow of fluid out of the eye, causing pressure in the eye to build. This pressure can damage the nerve that carries images from your eye to your brain (optic nerve).
“Diabetic retinopathy, macular edema, glaucoma or a combination of these conditions can lead to complete vision loss, if the conditions are poorly managed,” notes Dr. Bandara.
Treatment
In the early stages of diabetic retinopathy, controlling diabetes can help prevent vision problems developing. In more advanced stages, when a person’s vision is affected or at risk, keeping diabetes under control can help stop the condition getting worse. In case of diabetic retinopathy that is threatening or affecting a person’s sight, the main treatments include laser treatment, eye injections, steroid eye implants and eye surgery. “The majority of cases are managed with a combination of laser treatment and eye injections,” says the Eye Surgeon.
Retinal vein occlusion
Retinal vein occlusion is another condition to which people with diabetes are susceptible. Retinal vein occlusion is a partial or a total blockage in a vein that drains blood from the retina. The retina at the back of the eye is a layer of tissue which helps translate light into images. A blockage in a retinal vein prevents blood from leaving the retina and this could lead to complications including swelling of the macular and high eye pressure. Symptoms of retinal vein occlusion include blurry vision and floaters or dark spots or lines in the field of vision.
Retinal artery occlusion
 Retinal artery occlusion refers to blockage of the retinal artery carrying oxygen to the nerve cells in the retina at the back of the eye. The lack of oxygen delivery to the retina may result in severe loss of vision.
Retinal artery occlusion refers to blockage of the retinal artery carrying oxygen to the nerve cells in the retina at the back of the eye. The lack of oxygen delivery to the retina may result in severe loss of vision.
Ocular ischemic syndrome (OIS) although rare, is a vision-threatening condition people with diabetes are at the risk of. It is associated with severe carotid artery occlusive disease leading to ocular hypoperfusion. The symptoms include visual loss, transient visual loss, and ischemic ocular pain.
A presenile cataract
This is an early onset form of cataract that can develop in people as young as 40 years with diabetes. “It is believed that cataract is more prevalent and appears earlier in the diabetic population and the progress of the cataract is faster in such people compared to those with no diabetes,” says Dr. Bandara. He also points out that people with diabetes would often experience fluctuation in their spectacle strength. “When the blood sugar levels go up, they experience blurriness and feel their lenses won’t help, However, when the sugar levels come down, the vision will return to its former clarity.”
People with diabetes are also at risk of certain conditions that affect their optic nerve which is critical to vision. It is an extension of the central nervous system that includes the brain and the spine. It is the optic nerve which transmits electrical impulses from the eyes to the brain, enabling the brain to process the sensory information so that vision is possible.
Ischemic optic neuropathy is a condition where the blood vessels supplying to the optic nerve at its entry point to the eye get blocked. “Some people with diabetes could develop visual field defects affecting both eyes due to vision related nerves travelling along the brain that get damaged following a stroke. Diabetic papillopathy is another ocular complication of diabetes. It is characterised by optic disc swelling caused by vascular leakage and axonal edema in and around the optic nerve head.
They can get squints, double vision and even droopiness of the upper eyelids, due to either isolated nerve injury or as part of a stroke” explains the Consultant.
Diabetes could also increase the risk of glaucoma. “In the case of those with diabetes, their nerves are more vulnerable to eye pressure and PDR, complicated with neovascularisation of the iris” Dr Bandara explains.
Risk of infection
Diabetes affects the immunity of the body which makes people more prone to infections. “Even a small scratch in the eye or a foreign body in it like an insect falling for instance could cause infection very fast,” points out the Eye Surgeon who goes on to note that in case of such injury immediate proper medical care is needed without resorting to ad hoc treatment. “Even after immediate medical care, they need to be followed up to detect complications such as corneal ulcers early. A corneal ulcer is an open sore appearing on the cornea characterised by red, bloodshot eyes accompanied by a severe eye pain and eye discharge. Unless immediate care is given, this could lead to severe loss of vision. Other infections such as orbital cellulitis and black fungus (Mucomycosis) extending from adjacent sinuses need to be carefully attended to prevent vision loss and rarely, life threats.”
Poorly controlled diabetes could also affect the outcome of an eye surgery. “Be it cataract surgery or any other eye surgery, unless the sugar levels are controlled, the wound healing would take considerable time and there could be more post-surgical infection and post-surgical vision deteoration,” points out Dr. Bandara.
Early presentation and screening
Managing diabetes, hyper tension, cholesterol levels, anemia and ensuring proper renal functioning are critical for preventing diabetes-related eye complications and at the same time to manage the complications without making them worse. “Diabetic retinopathy, for instance, could be detected early with diabetic retinopathy screening. Annual screening of people with diabetes is essential to prevent loss of vision. In children diagnosed with diabetes, we do this screening around 12 years and thereafter annually to monitor them,” explains Dr. Bandara who reiterates the importance of seeking early eye care without resorting to ad hoc treatment or delaying treatment. “A good number of people seek medical care when the condition is too advanced and complicated and this could impact the success rate of treatment,” he added.