Sunday Feb 22, 2026
Sunday Feb 22, 2026
Monday, 8 January 2024 00:10 - - {{hitsCtrl.values.hits}}
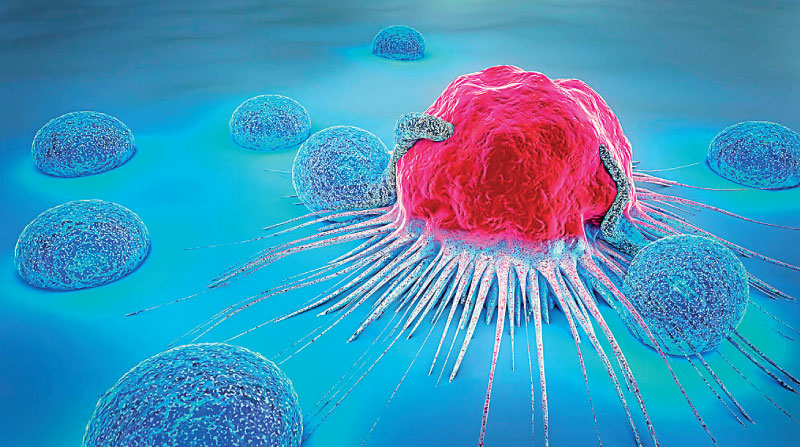
CAR T-Cell therapy is one of the most promising treatments for blood cancer
|
By Fathima Riznaz Hafi
|
Parkway Cancer Centre Singapore Senior Consultant Haematology Dr. Colin Phipps Diong
|
The notion of cancer, as nothing other than a death sentence, has come to pass over the years, with the advent of modern technology and innovations in medical science. Treatment for cancer has now come a long way, and numerous lives have been saved. However, there are certain types of cancer that are not fully treatable through existing methods. In such cases, even chemotherapy, a highly effective treatment for cancer, is not sufficient for complete cure. This is evident in the treatment of acute leukaemia – the most aggressive type of blood cancer.
Fortunately, new hope has arrived through a specialised and ‘targeted’ treatment called ‘Chimeric Antigen Receptor’ (CAR) T-Cell therapy, which is formulated to fight cancer cells more effectively. Parkway Cancer Centre Singapore Senior Consultant Haematology Dr. Colin Phipps Diong reveals that CAR T-Cell therapy is one of the most promising treatments for blood cancer. “Unlike with bone marrow transplants which use the cells of another person to fight cancer cells in the patient’s body, CAR T-Cell therapy is a process which involves using the patient’s own immune system to fight cancer. This immunotherapy treatment extracts the patient’s immune cells, known as ‘T cells’, which are then genetically altered in a lab to be used to locate and destroy cancer cells. This method is far more effective than other treatment methods for cancer, as it is a more targeted treatment, aiming directly at the cancer cells. It is the most advanced treatment for acute leukaemia,” he said.
Dr. Diong is a specialist in haematology, dealing with blood cancers like leukaemia, lymphoma, and myeloma. He was in Colombo recently to meet and discuss this new treatment, which is performed at Parkway Hospitals, with Sri Lankan doctors. In an interview with the press, he explains the unique nature of this method that enables it to take control of a severe case of leukaemia.
Acute leukaemia
“Acute leukaemia is the most aggressive type of blood cancer. Many children also have acute leukaemia. Now there is very good treatment for all these types of blood cancer and more than half the patients with acute leukaemia can be cured. Sadly, in some places that I go to give talks, I noted that for those patients, acute leukaemia is like a death sentence – they don’t know that they can be cured; but of course, that should not be the case because now there is a lot of treatment,” says Dr. Diong.
“Prior to this new treatment, most acute leukaemia patients were treated with a combination of chemotherapy and bone marrow transplantation. This transplant involves using cells from other people to fight the cancer cells.” Chemotherapy precedes bone marrow transplants.
Chemotherapy and bone marrow transplant
“Chemotherapy is not targeted treatment. It is very good treatment but it kills a lot of the fast growing cells in the body. For any cell that grows in the body very fast, chemotherapy will have the most effect on them. The fast growing cells include any sort of leukaemia or tumour (it is because they are fast growing, that they can grow into tumours), hair and skin. That’s why for chemotherapy the classic symptom is hair loss,” he explained, adding that this does not happen during CAR T-Cell therapy where only the cancer cells are targeted, and thereby healthy cells are spared.
The chemotherapy that is used for acute leukaemia is much more intense and stronger than when used for other types of cancer. “Because, when we do chemotherapy for leukaemia, what we want to do is directly target the cancer cells in that area; so we use chemotherapy, to affect the bone marrow production – for a while (few days). Each cycle, every time we give it, we see the patient’s white cell and red blood cell counts will drop a bit.
“We need to use strong chemotherapy so that we can kill all the bad cells in the bone marrow. While chemotherapy for breast, lung or liver cancer affects the bone marrow for a while, and is just a side effect, for acute leukaemia you actually want to target the bone marrow; so the intensity should be much higher,” he explained.
As a result, the side effects when treating acute leukaemia are much higher than when treating other types of cancer. The rate of severe infection and bleeding is also much higher.
The treatment period is very intense but very short.
A typical treatment for acute leukaemia would be strong chemotherapy – one cycle, two cycles, maybe three cycles – and then transplant. And that’s it.
CAR T-Cell therapy
CAR T-Cell therapy does not use chemotherapy at all. CAR T-Cell therapy tries to make your own immune cell kill the cancer cell directly. “But it’s a bit complicated – with chemotherapy, you just dilute the thing and then you infuse but with this procedure there is a bigger process – because in order to make your own immune cell directly kill the targeted cancer cell you have to collect T-cells from the patient’s blood. We can collect the red cell, white cell and also the T-cell. And we send what was collected, to the lab, which has to genetically engineer or modify the T-cell so that it can have the capacity to find the cancer cell and kill it. That is CAR T-Cell therapy,” Dr. Diong explained.
Once the lab makes it (it will take about five to eight weeks to make in the lab), they give it back to the patient and the T-cell will kill the targeted cancer cell.
This targeted treatment – CAR T-Cell therapy – is only approved for acute leukaemia and aggressive lymph node cancer (aggressive lymphoma).
Complete cure
Acute leukaemia presents very aggressively. “When you look at the patient’s symptoms you will be shocked; for example, they can have very low blood count and present very bad symptoms; they get very sick. But once we give the treatment, they can be completely cured,” Dr. Diong said.
The treatment takes a few months – it is very aggressive and fast. The recovery doesn’t take too long. Because with acute leukaemia being very aggressive, treatment must also be very aggressive – and fast, he explained.
Care during treatment
Dr. Diong noted that when it comes to patient care, especially for one suffering from acute leukaemia, the hospital staff must be very careful, because of the intensity of the treatment. The patient must be in a special type of single room where the air is flowing out from the patient’s room, rather than an open ward. In an open ward if a visitor has the flu, the patient also would get it and that is dangerous.
He added that the nursing staff has to be very cautious and clean – wear mask, wash hands thoroughly, etc.
Precautions like these need to be taken because the patient can die from infection, he warned.
“Very simple precautions – hygiene in the ward – wear mask, doctors, nurses wash hands after every patient. My hands turn red and skin peels after all the alcohol rubs – but I still do it – it’s not difficult. Simple steps in hygiene,” he said.
Food
Dr. Diong said that during treatment, it is important to guide the patients on what to eat and what not to eat. Very intensive treatment makes the patient’s immune system very weak (for a while – until they recover); so during that time, the food must be very clean, and very well-cooked. “Like for my patients who undergo very intensive treatment, I don’t even let them eat salad, because it’s raw. No uncooked food. Vegetables are fine if cooked. I know we lose some of the nutrients when they are cooked, but too bad, it must be done; everything has to be well-cooked, to be safe. Even with milk, when you buy milk, you can keep and use it for one or two days but not beyond that. Overnight food cannot be eaten. Home-cooked food is ideal but if they need to eat out, they have to be very careful when choosing as they don’t know how fresh the food is.
“Of course, when the immune system is back to normal and once the patient has fully recovered, they can go back to eating what they want,” he said.
Parkway is the first private hospital in Singapore to be given approval to practice CAR T-Cell therapy, and it was initiated by Dr. Diong. It is common in other countries like US, UK, Japan, Saudi Arabia, and Australia, but this treatment is not available in Sri Lanka yet. Dr. Diong will be coming to the country frequently to speak to and support local doctors, and discuss case studies and treatment.