Friday Feb 20, 2026
Friday Feb 20, 2026
Tuesday, 18 May 2021 00:00 - - {{hitsCtrl.values.hits}}
|
With the rapidly-increasing incidence of COVID-19 in Sri Lanka and the health systems’ possible inability to provide in-hospital care for PCR-positive COVID-19 patients, the home as a setting for clinical care provision for asymptomatic mild COVID-19 patients may indeed become possible or even necessary. In this context, pre-emptive planning for provision of home-based care for carefully clinically-triaged and selected patients becomes important – Pic by Shehan Gunasekara |
Most people with COVID-19 develop mild or uncomplicated illness that can be managed at the primary care level, and the demand for primary care services will escalate during periods of increased transmission.
Health policymakers at the national and subnational level will need to take appropriate action to support the role of primary care in the response, such as managing mild COVID-19 cases or recovery of hospitalised cases, identifying strategies to increase surge capacity, managing and maintaining stocks of personal protective equipment (PPE) and other essential supplies, and maintaining of essential services, while ensuring timely adaptation to address the needs of vulnerable groups.
With the rapidly-increasing incidence of COVID-19 in Sri Lanka and the health systems possible inability to provide in hospital care for PCR positive COVID-19 patients, the home as a setting for clinical care provision for asymptomatic mild COVID-19 patients may indeed become possible or even necessary. In this context pre-emptive planning for provision of home-based care for carefully clinically triaged and selected patients becomes important.
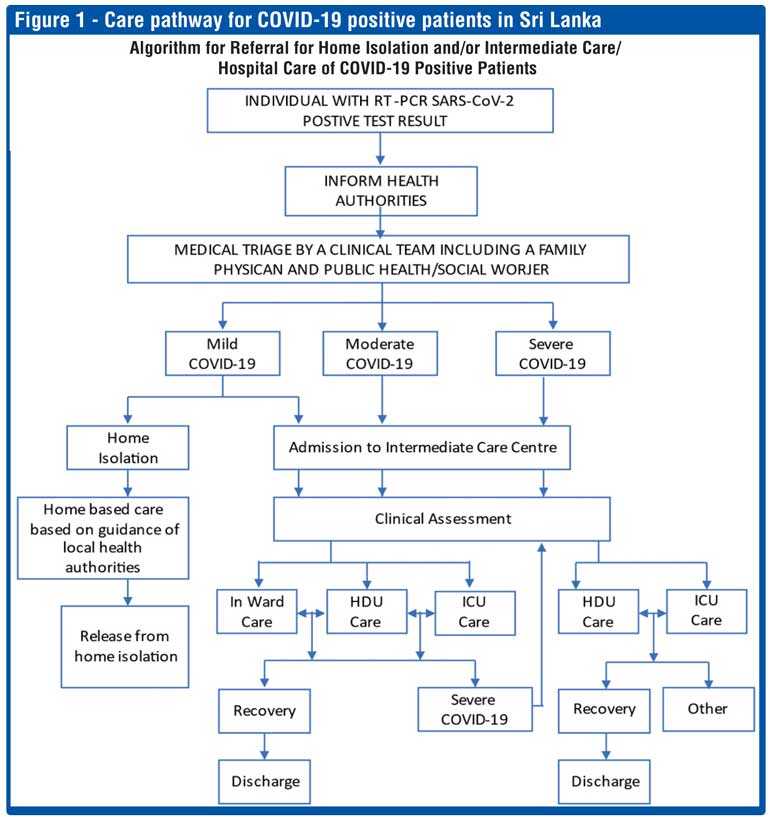
As per the WHO, COVID-19 is classified into three clinical entities – mild, moderate, and severe (Fig.1). People classified as having mild COIVID-19 with no symptoms should be able to stay at home, if adequately isolated from others. This also implies that if you are symptomatic even with mild COVID-19 you will require hospital admission.
Decision to care for COVID-19 patients at home
This decision cannot and should not be made by the patient or the family. This decision must be made after clinical triage by a healthcare team which must include a family physician and social worker who is aware of the patient’s physical home infrastructure in addition to the past and current health status of the patient.
 Home care should be considered for an adult or child with confirmed COIVD-19 when in patient care is unviable or unsafe (e.g. when heath care service capacity is insufficient). It must be understood that home care increases the risk of transmitting the virus to others at home. However, isolation of people at home and using the home as a clinical setting to provide care to carefully selected patients can make an important contribution to breaking the chain of transmission of the virus.
Home care should be considered for an adult or child with confirmed COIVD-19 when in patient care is unviable or unsafe (e.g. when heath care service capacity is insufficient). It must be understood that home care increases the risk of transmitting the virus to others at home. However, isolation of people at home and using the home as a clinical setting to provide care to carefully selected patients can make an important contribution to breaking the chain of transmission of the virus.
Home care (provided requirements are fulfilled) should ideally be considered for individuals under the age of 60 years, do not smoke, are not obese and have no other diseases such as cardiovascular diseases, diabetes mellitus, chronic lung disease, cancer, chronic kidney disease or immune suppressed.
The decision to isolate and care for an infected person at home depends on the following three factors:
1. Clinical evaluation of the COVID-19 patient
2. Evaluation of the home setting (see box 1). In the Sri Lankan context of considering home as clinical setting for COVID-19 home care the following in addition to box 1 should also be considered.
2.1. Adequate floor space area with minimum two individual rooms, adequate natural ventilation and two toilets
2.2. Home should preferably have access to running water.
2.3. The infected patient/family should be equipped with communication facilities to contact healthcare providers routinely and in an emergency.
3. Ability to monitor the clinical evolution of the person at home.
What to monitor in a COVID-19 positive patient receiving home care
The patient and care giver must be advised about the signs and symptoms of complications or how to recognise deterioration in their health status that requires medical attention.
The most important parameters to monitor in the home setting are fever, difficulty in breathing, fast or shallow breathing, blue lips or face, chest pain or pressure, confusion (which was not present earlier), inability to wake up, inability to interact when awake and inability to drink or keep liquids down. For infants in addition to these, grunting and inability to breastfeed also must be considered. (Please note this list is not an exhaustive list and if you have any doubt, please contact healthcare team immediately.)
Home pulse oximetry is a safe, non-invasive way to assess oxygen saturation in the blood and can support the early identification of low oxygen levels in patients with initially mild or moderate COVID-19 or when patient does not appear short of breath but their oxygen levels are lower than expected (silent hypoxia). Home pulse oximetry can identify individuals in need of medical evaluation, oxygen therapy or hospitalisation, even before they show clinical signs of worsening signs or symptoms.
This writer is of the view that if home care for mild asymptomatic COVID-19 positive patient is recommended the minimum requirement should also include the possession or access to a finger pulse oximeter.
What should be done to prevent other people in the house from becoming sick if a person with COVID-19 is being cared for at home?
It is highly recommend that the patient, caregiver/s are given a simple and short orientation program to use the provided equipment and to create awareness on the ‘red flag’ signs to look out for and contact the primary healthcare provider for further instructions.
There are several precautions that can prevent the spread of COVID-19 to other people in the house:
The ill person should stay in a separate room. If this is not possible, then keep at least a one-metre distance from them. The sick person and anyone else in the same room should wear a medical mask.
Provide good ventilation in the room of the ill person and shared spaces, and open windows if possible and safe to do so.
The ill person should wear a medical mask as much as possible, in particular when not alone in the room and when at least a one-metre distance from others cannot be maintained. Limit the patient’s movement around the house and minimise shared spaces. Ensure shared spaces (e.g. kitchen, bathroom) are well ventilated.
Visitors should not be allowed in the home.
Limit the number of caregivers to one person with no underlying conditions, if possible.
Caregivers and household members should wear a medical mask while in the same room with an ill person, not touch their mask or face during use, discard the mask after leaving the room, and wash their hands afterward.
The ill person should have dedicated dishes, cups, eating utensils, towels and bed linens. They should be washed with soap and water, and not shared.
Frequently touched surfaces by the ill person should be cleaned and disinfected at least daily.
Everyone in the household should wash their hands with soap and water regularly, especially:
after coughing or sneezing
before during and after you prepare food
before eating
after using the toilet
before and after caring for the ill person
when hands are visibly dirty
A cough or sneeze should be covered with a flexed elbow or a disposable tissue that is discarded immediately after use.
The waste from the ill person should be packed in strong closed bags before disposal.
The household (patient and care giver/s) should be encouraged to have steady supply of masks (essential, three-ply surgical mask would do), face shield (optional), disposable or washable overalls (optional), 70% alcohol hand sanitiser (optional in the presence of clean running water and soap)
How long should people with COVID-19 stay at home and in isolation?
People with COVID-19 who are cared for at home should stay in isolation until they are no longer able to transmit the virus to others.
Those with symptoms should stay isolated for a minimum of 10 days after the first day they developed symptoms, plus another three days after the end of symptoms – when they are without fever and without respiratory symptoms.
People without symptoms should stay isolated for a minimum of 10 days after testing positive.
Please check with your family physician/PHI for updated release from home isolation guidelines as they subject to update.
Conclusion
Primary care is an essential foundation for the global response to COVID-19. Primary care plays a significant role in gatekeeping and clinical responses: identifying and triaging possible COVID-19 cases, making an early diagnosis, helping vulnerable people cope with their anxiety about the virus, and reducing the demand for hospital services.
The role of primary care has been increasingly important as cities imposed strict control measures including non-pharmaceutical interventions and as larger hospitals closed their outpatient departments during periods of increased transmission.
There also is an increasing role of home care for COVID-19 cases within communities supported by a strong primary care system, which strengthens the trust between health-care workers and communities. A response built around primary care has also been a more cost-effective measure.
The SARS-CoV-2 Virus is doing its job. Are we as individuals, families and communities doing our job to prevent the spread of the virus? None of us will be safe until all of us are safe.
The Government/health authorities by allowing the home care of mild asymptomatic COVID-19 patients are taking us the people of Sri Lanka into their confidence and giving us responsibility to actually be part of the clinical care process of COVID-19 management in Sri Lanka. Let us not disappoint the Government/health authorities by misusing, manipulating, and abusing the trust they have placed in us. Let us show them that we the people of Sri Lanka if given responsibility will deliver on it in the context of home care for COVID-19 patients.
References
1. Home care for patients with suspected or confirmed COVID-19 and management of their contacts. Interim guidance 12 August 2020. Updated 2 March 2021.
2. Role of primary care in the COVID-19 response. Interim guidance. Revised and republished as of 9 April 2021 (Originally published 26 March 2020).
The writer is a Family Physician, Head of Dept. of Family Medicine, Faculty of Medicine, University of Colombo and Past President of Sri Lanka Medical Association
Factors to consider when assessing home as clinical setting for COVID-19 care
|