Monday Feb 23, 2026
Monday Feb 23, 2026
Saturday, 10 December 2016 01:22 - - {{hitsCtrl.values.hits}}
By Samanthi Bandara
The global development framework has evolved to be more inclusive beyond 2015, with the integration of Sustainable Development  Goals (SDGs) in economic, social, and environmental aspects. ‘Health’ with regard to achieving Universal Health Coverage (UHC), takes notable recognition in linking to the goals in the sustainable development agenda.
Goals (SDGs) in economic, social, and environmental aspects. ‘Health’ with regard to achieving Universal Health Coverage (UHC), takes notable recognition in linking to the goals in the sustainable development agenda.
It is well-known that Sri Lanka is placed much ahead in terms of health outcomes compared to neighbouring countries. However, regional disparities remain. This is further aggravated by the demographical (health of ageing population) and epidemiological transitions, as well as the country’s move towards a high-income level. Conversely, financial insecurity when it comes to seeking care has arisen because of public health services that are inadequate in quality and quantity. This in turn has created an increase in out of pocket expenditure.
In this context, the emergence of the sustainable development agenda, subsequent to the Millennium Development Goals (MDGs), with a comprehensive and exclusive goal for health opens another window to set the newest targets and respective actions towards UHC.
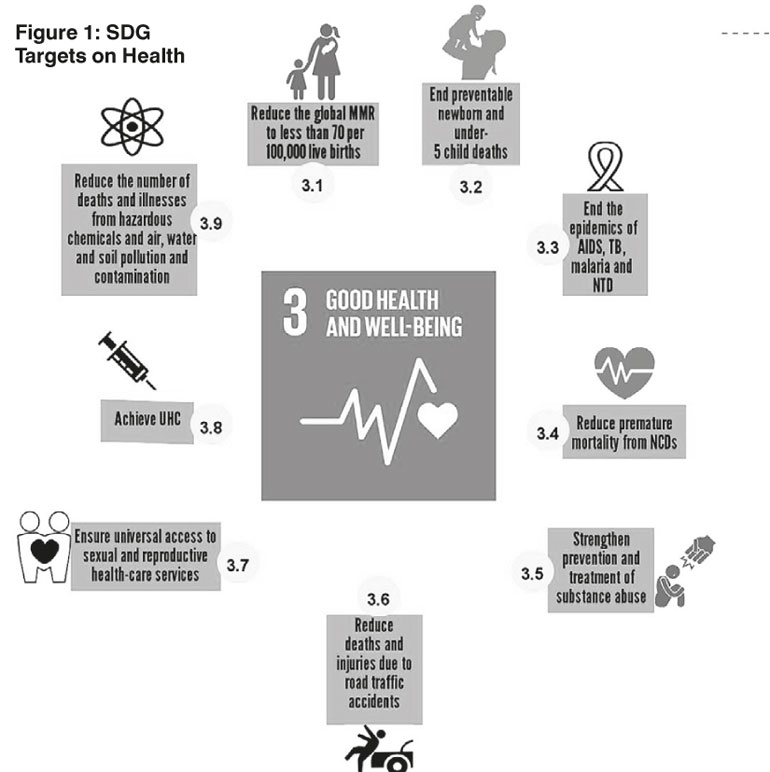
Subsequent to the MDG agenda, the 17th anniversary of the UN Assembly embarked on a new vision, which is the 2030 Agenda for SDGs. This introduced 17 goals and 169 targets, of which, Goal 3 comprising 9 sub-goals and 4 implementation goals are assigned for health with an aim to “ensure healthy lives and promote well-being for all at all ages” (Figure 1). So far, more than 15 indicators are identified to measure the outcomes of the set goals.
While the MDGs were exclusively framed to strengthen human development, SDGs go beyond this, capturing a wider spectrum on economic, social, and environmental dimensions. This integration is the key to making health in SDGs critically different from other development agendas. One can argue that the first three SDG health sub-goals (Figure 1) are to continue MDG targets further. This is correct, as the said three sub-goals still exist to point out crucial areas of a country’s health outcomes.
The focus of SDGs is not limited to diseases. It also sets insistent targets towards reducing inequity in health within and between societies, with an emphasis on UHC, which identifies the determinants of health within and beyond the health sector. As such, SDG 3.8 on “achieving universal health coverage” is a platform, which incorporates all other sectors, reinforcing the existing approach on “health in all policies”.
Making commitments towards UHC via SDG is commendable, but it can only be successful if the following two factors can be accomplished. Firstly, UHC can be achieved once the dimensions of health service coverage, financial protection, and population coverage are cumulatively addressed. Secondly, intersectoral collaborations/actions with other SDG goals, namely, poverty reduction (Goal 1), provision of water and sanitation (Goal 6), urbanisation and service delivery in human settlement (Goal 11), provide a perfect complement towards achieving UHC. Besides, the SDG agenda has explicitly stated the need to take steps towards ensuring equity by phrasing that “no one will be left behind”.
The SDGs have also envisioned addressing health system issues in terms of supporting health research and development, increasing health financing, strengthening human resources, and increasing capacities for risk reduction and risk management through ‘implementation targets’.
Within the South Asia region, Sri Lanka’s health system has been well ahead to sustain basic health outcomes. This is also highlighted in the 3rd MDG report. However, the country still needs advanced interventions to smoothen the drive towards basic health outcomes.
For instance, Sri Lanka has already met the universally agreed upon SDG targets in terms of maternal mortality, neonatal mortality, and under 5 mortality. However, these targets are only being achieved at national level and regional disparities persist. As such, the continuation of MDG health targets through SDG 3.1 and 3.2 are still pertinent.
Even though Sri Lanka is free from a few infectious diseases (e.g., Malaria, Filariasis), some of the diseases, particularly HIV, Dengue, and TB are on the rise. Accordingly, SDG 3.3 on infectious diseases can still contribute to Sri Lanka’s health sector improvements, towards implementing target-oriented interventions to combat such diseases.
NCDs and mental health issues are on the rise, and are the leading causes of deaths in Sri Lanka, accounting for 75% of all deaths, while 14% of deaths occur due to injuries. Meanwhile, ischaemic heart disease has become the leading cause of hospital deaths in the country.
Further, premature mortality – deaths between the ages of 30 and 70 – stands at 18 people out of 100 in the country. Moreover, mortality due to NCD is projected to increase in the coming years with high exposure to NCD risk factors (i.e., exposure to agricultural and industrial chemicals, unhealthy food habits, use of alcohol and tobacco) despite demonstrating a relative reduction in the previous years.
To combat the said epidemic, the country has already taken measures by implementing a NCD National Policy, and ‘National Multisectoral Action Plan for the Prevention and Control of NCDs 2016-2020’. Therefore, SDG 3.4 – 3.6 and 3.9 can complement the national initiatives on NCDs, which can then accelerate NCD prevention and control.
SDG 3.7 on ‘ensuring universal access to sexual and reproductive health-care services’ is already consistent with Sri Lanka’s national targets. To this end, it is crucial to give priority to reducing teenage pregnancies, unsafe and illegal abortions, and increasing contraceptive prevalence rate.
An inadequate and inequitable public health service is one of the crucial factors, which create inequity in health outcomes in the country. Such a situation then impels people to seek alternative health care services, particularly by moving towards the private health sector. A majority of people does not have health insurance, and pay for the services out of their pocket.
Meanwhile, a majority of the people is financially insecure and that is further underlined by the high rate of out of pocket expenditure on health (OOP). Besides, inequity in health outcomes is also persistent. Accordingly, ensuring equity in health outcomes is pivotal for Sri Lanka and which can be addressed by the SDG on UHC.
Technically, there is no doubt that SDG Goal 3 is relevant to Sri Lanka. However, Sri Lanka has the responsibility of making adjustments to SDGs to suit the country, but within the given framework. It is important to form an institutional mechanism (apex-body) with a strong political commitment, which can ensure effective planning, implementation and monitoring of SDGs.
The SDGs should also be prioritised to be aligned with national health policy initiatives through proper financing estimates, and monitoring and evaluation systems at regional and national levels. Importantly, setting up a coordination mechanism between health and beyond the health sector is vital to ensure that overlaps and duplications do not occur.
Next, the biggest bottleneck is finding financial, physical, and human resources and employing them in an effective and efficient manner. The estimated cost for achieving SDGs, particularly in developing countries is in the range of $ 3-7 billion per year, and every year a gap of $ 2.5 billion remains. However, a clear funding source has not been identified.
Even for Sri Lanka, increasing fiscal space is tricky when looking at the current spending on health. Even achieving UHC requires 5% of GDP on health, and reducing OOP to below 40% of the total health spending. Therefore, Sri Lanka has to make a significant effort to be financially secure before starting the SDG agenda.
Prior to seeking funds from outside, the country can peruse opportunities through the private sector as done by other neighbouring economies (e.g., Singapore, Malaysia, and Thailand). This can be done through public-private partnerships. In addition, reorienting the existing resource allocation mechanisms to align with SDG targets would also open avenues to fill the required additional resources. Implementing the agreed SDG agenda may not be straightforward. However, the country can start the implementation of SDG 3 by making suitable amendments within the present system.