Sunday Feb 22, 2026
Sunday Feb 22, 2026
Thursday, 20 June 2019 00:00 - - {{hitsCtrl.values.hits}}
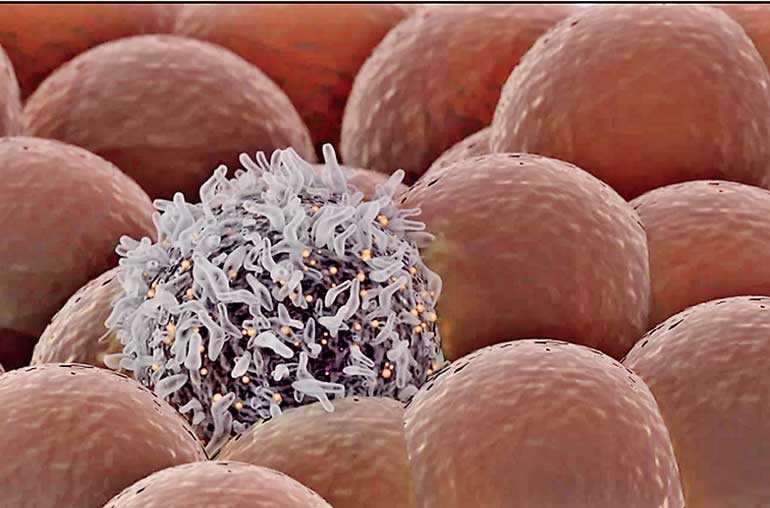
livescience.com: Cancer cells can spread to other parts of the body through the blood. And now, researchers have developed a new kind of laser that can find and zap those tumour cells from the outside of the skin.
Though it may still be a ways away from becoming a commercial diagnostic tool, the laser is up to 1,000 times more sensitive than current methods used to detect tumour cells in blood, the researchers reported 12 June in the journal Science Translational Medicine.
To test for cancer spread, doctors typically take blood samples, but often the tests fail to find tumour cells even if they are present in a single sample, especially if the patient has an early form of cancer, said senior author University of Arkansas for Medical Sciences Nanomedicine Centre Director Vladimir Zharov.
If the tests do come back positive, that typically means there's a high concentration of circulating tumour cells in the blood; at that point, the cancer has likely spread widely to other organs and it's often “too late to effectively treat patients”, Zharov added.
Years ago, Zharov and his team came up with the idea of an alternate, non-invasive method to test larger quantities of blood with a greater sensitivity. Taking the familiar route, they tested it in the lab, then on animals and recently brought it to clinical trials in humans.
The new technology, dubbed the Cytophone, uses pulses of laser light on the outside of the skin to heat up cells in the blood. But the laser only heats up melanoma cells – not healthy cells – because these cells carry a dark pigment called melanin, which absorbs the light. The Cytophone then uses an ultrasound technique to detect the teensy, tiny waves emitted by this heating effect.
They tested the technology on 28 light-skinned patients who had melanoma and on 19 healthy volunteers who didn't have melanoma. They shone the laser onto the patients' hands and found that within 10 seconds to 60 minutes, the technology could identify circulating tumour cells in 27 out of 28 of those volunteers.
Finding and killing tumour cells
The device didn't return any false positives on the healthy volunteers, and it didn't cause safety concerns or side effects, they said. Melanin is a pigment that is normally present in the skin, but skin cells aren't harmed, Zharov said.
Even though the skin produces melanin naturally, this laser technique doesn’t harm those cells. That’s because the laser light exposes a relatively a large area on the skin (so it's not focused enough on individual skin cells to damage them), while the laser energy is more concentrated on the blood vessels and circulating tumour cells, he added.
Unexpectedly, the team also found that after the treatment, the cancer patients had fewer circulating tumour cells. “We used a relatively low energy” with the primary purpose of diagnosing rather than treating the cancer, Zharov said. Yet, even at that low energy, the laser beam seemed able to destroy the cancer cells.
Here’s how it works: As the melanin absorbs the heat, the water around the melanin inside the cells begins to evaporate, producing a bubble that expands and collapses, mechanically destroying the cell, Zharov said.
“Our goal is by killing these cells, we can help prevent the spreading of metastatic cancer,” he said. But he hopes to conduct more research to optimise the device further to kill more tumour cells, while still being harmless to other cells.
They also haven't yet tested the device on people with darker skin, who have higher levels of melanin. Even so, only a very small percentage of African-Americans get melanoma. The team hopes to expand the technology to find circulating tumour cells released by cancers other than melanoma. These cancer cells don't carry melanin, so to detect them, the researchers would first need to inject the patients with specific markers or molecules that would bind to these cells so that they can be targeted by the laser. They have so far demonstrated that this technique could work on human breast cancer cells in the lab.