Wednesday Feb 18, 2026
Wednesday Feb 18, 2026
Friday, 16 November 2018 00:00 - - {{hitsCtrl.values.hits}}

By Sonalini Khetrapal
blogs.adb.org: In 2017, a record 123 million children were immunised globally. Immunisation is one of the most cost-effective public health interventions, averting an estimated two to three million deaths every year.
Effective immunisation programs have led to a world closer to eradicating polio than ever, while measles vaccination has resulted in an 84% drop in deaths during 2000-2016. Last year, global coverage rates for the third dose of the diphtheria, tetanus, and pertussis vaccine (DTP3) reached 85%.
Despite these achievements, progress on immunisation has stalled in the current decade.
As of August 2018, 71 countries have yet to achieve the Global Vaccine Action Plan target of 90% or greater coverage of DTP3. In 2017, 19.9 million children under one did not receive the full three recommended doses of DTP3, and 20.8 million children were denied a single dose of measles vaccine.
Significant efforts and resources are dedicated to supporting, maintaining, and improving immunisation strategies to achieve the goals set by national and international health agencies. One of these is to achieve and maintain appropriate vaccine coverage to successfully control and eliminate vaccine-preventable infectious diseases.
However, maintaining a high-performance immunisation program is one of the most challenging public health objectives.
A number of issues have become real threats for maintaining coverage, running effective surveillance, and allowing immunisation programs to react in a timely manner to new problems. These include logistics management, underreporting and under-recognition of adverse effects following immunisation, reduction of public confidence in vaccinations, and lack of effective communication strategy for vaccine promotion.
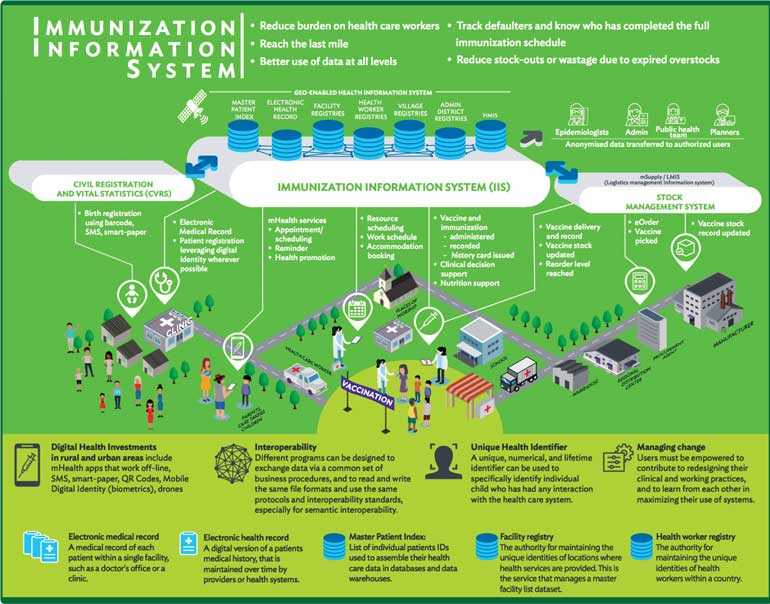
One way forward is to adopt rapidly developing digital health tools that offer solutions to improve service delivery.
Digitisation can help boost providers’ capability to make immunisation health value chains more efficient and resilient. While efficiency improvements arising from streamlined resource flows result in additional funds for possible investments to improve service delivery, resilience needs redundancy for enhanced capacity and diversity to respond effectively to risks such a stock-outs for both supplier and user.
Digital tools are highly productive in several vaccine-related areas:
For improved decision support systems, leading to effective and efficient service deliver, GIS is a powerful tool to identify gaps and inequities in access to immunisation services, and to support better decision making around targeting immunisation resources. It helps integrate, visualise and analyse data on immunisation resources, population distribution and the connecting geographic environment (e.g. transport network, geographic barriers), as well as model accessibility to health services.
In a resource constraint settings, better integration of immunisation information system and CRVS (Civil Registration and Vital Statistics) data architecture has the potential to provide transformative improvements in both systems. Among these are streamlining and extending registration coverage, integrating data from multiple systems, and securely storing data at scale – all in a cost-effective way.
For example, health workers, by virtue of their extended reach, can notify civil registrars of births/deaths. In turn, health programs benefit from fully functioning CRVS data because it makes real-time data available to expand immunisation coverage.
A digital architecture is essential to attain interoperability between health programs, CRVS, and related systems such as unique health identifiers.
Interoperability requires developing protocols to share information and data. This covers master patient indexes, electronic health records and registries, health management information systems, health IDs, and population censuses, to name a few.
To achieve interoperability, it is imperative to work with communities to address issues of confidentiality, privacy, and data security within a sound legal and governance framework. Joint capacities and human resources need to be developed to implement the innovations.
For instance, training materials can be adopted to diverse settings alongside institutional mechanisms for capacity development, with a particular focus on immunisation and CRVS interoperability. Social workers, case managers, school employees, and community health workers must be trained on notifications of births/deaths to ensure these are officially registered according to international standards.
Finally, a logistics management information system (LMIS) provides data on vaccine supply and demand, which can be used to reach more children with greater efficiency.
As vaccines become more expensive and demand greater storage capacity at every level of the cold chain, countries must keep lower stock levels, reduce wastage, accurately forecast vaccine requirements, and prevent equipment failure. This requires a consistently high standard of supply chain management, which can only be achieved if all the links comply with current standards for storage and distribution.
Digitisation can improve LMIS via standardised data collection, quick data transmission throughout the system, error reduction, and automated reports that elucidate the best course of action. Strong vaccine supply chains ensure that children have access to the right vaccines, at the right time, in the right place.
(The writer is Health Specialist, Sustainable Development and Climate Change Department, ADB.)