Thursday Feb 19, 2026
Thursday Feb 19, 2026
Thursday, 28 September 2017 00:34 - - {{hitsCtrl.values.hits}}
 Some may still remember an incident that made news in September 2015; a popular private hospital in Colombo agreed to undertake a heart by-pass operation for Rs. 700,000 and accepted Rs. 300,000 as an advance. A few days after the operation, the patient’s condition took a bad turn and the patient died.
Some may still remember an incident that made news in September 2015; a popular private hospital in Colombo agreed to undertake a heart by-pass operation for Rs. 700,000 and accepted Rs. 300,000 as an advance. A few days after the operation, the patient’s condition took a bad turn and the patient died.
According to the hospital the charges amounted to over Rs. 2.1 million due to the extended treatment. The hospital refused to release the deceased body and the relatives had to seek Police assistance and finally the court ordered the body be released.
A couple of years ago, a friend of my son, a young man in early thirties, married with a child, employed with a private organisation, and parents, retired teachers from Amparai were living with the family. The young man’s mother had a stroke and was admitted to a private hospital. The
doctors diagnosed the problem to be ruptured blood vessel in the brain. They informed the son that the mother required immediate brain surgery, which would be expensive and had a 5% possibility of success.
The family was not rich, but the son agreed to the surgery. His argument was, if I were placed in such a situation, what would my parents do? The surgery was performed, the mother regained consciousness and was able to recognise the son, unfortunately the mother passed away a few hours later. The son had to face a hospital bill of Rs. 1.8 million and the hospital refused to release the body until the bill was settled. The young man had to sell his only possessions, a car and a motorcycle, to settle the bill.
Private hospitals and their administrators have not changed, in fact things have got worse. The recent dengue epidemic was a Godsend for private hospitals. When a person got flu and high temperature continued for two to three days, family members rushed the patient to the hospital. Although the dengue test takes only a few hours, hospitals carry out series of unnecessary other tests, consultants are brought in and when the patient is discharged in a few days, the bill has reached several hundreds of thousands.
What is a Living Will?
A Living Will, also referred to as an advance directive, is a legal document that provides instructions regarding end-of-life care, when the person does not have the capacity to make decisions or not in a condition to communicate own wishes due to illness or incapacity. A Living Will allows one to make own choices about life support in advance and helps prevent confusion about the type of care you expect or do not want in the event you become incapable of communicating your wishes.
A Living Will provides specific directives about the course of treatment to be followed by health care providers and caregivers for medical treatment in the event of a terminal illness, an injury, or permanent unconsciousness. In some cases a Living Will may forbid the use of various kinds of burdensome medical treatment. It may also be used to express wishes detailing your preferences for tube feeding, artificial hydration and pain medication in certain situations. A Living Will becomes effective only when you cannot communicate your desires.
A Living Will can be very specific or very general. An example of a statement sometimes found in a living will is: “If I suffer an incurable, irreversible illness, disease, or condition and my attending physician determines that my condition is terminal, I direct that life-sustaining measures that would serve only to prolong my dying be withheld or discontinued.”
When a person is unable to communicate desires in such situations and without a Living Will, doctors or hospitals may decide they are legally obliged to perform certain procedures that you would not desire, but increase their financial gain. If the spouse, adult child or another relative is called to decide about your care, decision would be easy and helpful if the Living Will has expressed your wishes. A Living Will tells others what you want to happen under such circumstances.
Typical forms for Living Wills are available over the internet mostly from the US. More specific Living Wills may include information regarding an individual’s desire for such services such as analgesia (pain relief), antibiotics, hydration, feeding, and the use of ventilators or cardiopulmonary resuscitation. However, studies in the US have also shown that adults are more likely to complete these documents if they are written in everyday language and less focused on technical treatments.
By planning ahead, you can get the medical care you want, avoid unnecessary suffering and relieve caregivers of decision-making burdens during moments of crisis or grief. The Living Will also helps to reduce confusion or disagreement about the choices you would want your loved ones to make on your behalf.
Living Will vs. Last Will
The Living Will should not be confused with a Last Will. A Last Will and Testament express what you want to happen to your property and minor children in the event of your death. A Living Will expresses what you want to happen to your person regarding medical treatment while you are still alive, but in a condition you are unable express your wishes.
Revoking or cancelling a Living Will
If you execute a Living Will and later create a new Living Will, it can be done in two ways. First, you can revoke the previous Living Will. A Living Will can be cancelled or revoked at any time. You can cancel your Living Will by indicating, in writing, that it has been cancelled. Destroying your original Living Will may cancel the will, but revoking the will in writing is more formal. Second, you can execute a new Living Will that expresses your current desires. This has the effect of cancelling your previous Living Will. The revocation is effective when you, your proxy, or someone else who witnessed your revocation communicate it to your attending physician or healthcare provider.
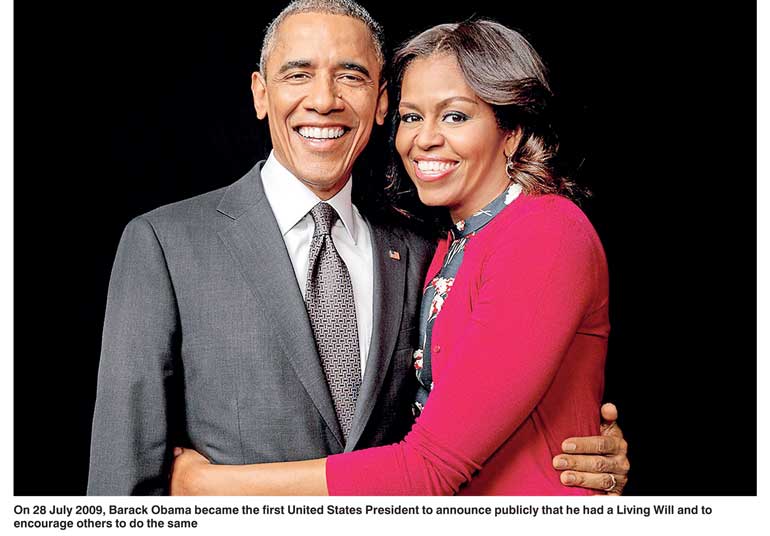
Living Will and President Obama
Living Wills proved to be very popular in United States, and by 2007, 41% of Americans had completed a Living Will. On 28 July 2009, Barack Obama became the first United States President to announce publicly that he had a Living Will and to encourage others to do the same. He told at a town meeting, “So I actually think it’s a good idea to have a Living Will. I’d encourage everybody to get one. I have one; Michelle has one. And we hope we don’t have to use it for a long time, but I think it’s something that is sensible.”
Patient Self-Determination Act
In the US, hospitals, nursing homes and home health agencies come under a federal law called the Patient Self-Determination Act (PSDA) are required provide information on advance directives at the time of admission. The PSDA simply requires that most health care institutions (but not individual doctors) do the following:
1. Give you at the time of admission a written summary of your health care decision-making rights.
2. Ask you if you have an advance directive, and document that fact in your medical record if you do. (It is up to you to make sure they get a copy of it).
3. Educate their staff and community about advance directives.
4. Never discriminate against patients based on whether or not they have an advance directive. Thus, it is against the law for them to require either that you have or not have an advance directive.
The origin
The Living Will originated in the United States as a response to the increasing sophistication and prevalence of medical technology and the ability of medical institutions to deliberately to delay death. It has been found that the patient’s death has been unnecessarily prolonged resulting painful, expensive, and emotionally burdensome to both patients and their families. Currently Living Will or similar legislation has been enacted in large number of other countries including UK, Canada, Australia, Switzerland, Germany, Netherlands and others.
The advances of medical technology backed by some religious groups who claim of some historic instances, where individuals at death-bed were rescued by some miraculous ways and / or by their faith on some God. Thus, they claim individuals may be rescued at the last moment of death and none has the right to advance death.
In developed countries majority of people are insured and the insurance companies foot hospitalisation bills. The doctors and medical institutions made undue advantage of the situation for unfair financial gain. But other groups fought back against unjustified money making of medical institutions resulting populace signing the Living Will.
In the US, the Patient Self-Determination Act (PSDA) came into effect in December 1991, and required healthcare providers (primarily hospitals, nursing homes and home health agencies) to give patients information about their rights to make advance directives under state law. Living wills proved to be very popular, and by 2007, 41% of adult Americans had completed a Living Will.
Are Living Wills only for old people?
It is true that older, rather than younger, people subscribe to Living Wills, but every adult should have one. Younger adults actually have more at stake, because, if stricken by serious disease or car accident, medical technology may keep them alive but in an unconscious state for decades.
Does a Living Will mean “do not treat”?
A Living Will can express both what you want and don’t want. It does not assume “do not treat”. Even if you do not wish treatment to cure you, you should always be kept reasonably pain-free and comfortable.
The healthcare proxy
A healthcare proxy (durable power of attorney) is a document that names someone you trust to make health decisions when you can’t. A Living Will tells which treatment you want if your life is threatened, including: dialysis and breathing machines, resuscitation if you stop breathing or if your heart stops, tube feeding, organ or tissue donation after you die.
Naming a proxy
Your proxy could be wife/husband son/daughter or any other trustworthy individual. Naming a health care proxy or agent does not take away any of your authority. You always have the right, while you are still competent, to override the decision of your proxy or revoke the directive.
What to do with your Living Will
1. Keep the original copies of your Living Will where someone can easily find it.
2. Give a copy to your healthcare proxy, healthcare providers, hospital, nursing home, family, and friends.
3. Carry a card in your wallet that says you have a Living Will.
4. Review your Living Will each year.
Donation of organs
For a long period Sri Lankans signed documents indicating willingness to donate their eyes after death. Recently our doctors succeeded transplanting a heart from a clinically dead person to a living recipient. Also transplanting other organs as kidneys is becoming common and newspapers carry advertisements requesting possible donors. This opened doors to a complete unopened opportunity of donating and transplanting organs.
But the biggest challenge is to find persons willing to donate. Young persons executing their Living Wills could solve the problem. They could indicate the willingness to donate organs, tissues, or eyes for the purpose of transplantation, therapy, medical research, or body for anatomical study if needed or limitations or special wishes, if any, and carry a card in their wallets indicating presence of a Living Will.
Elders in Sri Lanka
Every Government so far has washed its hands off senior citizens claiming “looking after elderly is the responsibility of the children”. Most married couples live away from parents due to their employment, also for children’s schooling. But some live in their parent’s house and parents help to look after young. But as children grow up, parents become feeble and need looking after, a difficult situation especially when servants are expensive. Modern upstairs houses, built on small plots of land, restrict elders from walking for fitness, making the situation worse.
In upper society children are sent abroad for further education and get settled, leaving parents alone at home, who get trapped in their own houses. They become feeble, paid carers who could cost upwards of Rs. 1,750 for a 12-hour shift and food costing over Rs. 100,000 a month forces them to move into a specialist care home.
Elders’ homes
Current elders’ homes cover a wide range from entirely free (depending on public alms for food) and some get donations from abroad, to nominally paying to high end. The service would vary depending on charges.
Final sickness
Most elders suffer from diabetes, high blood pressure and other ailments which are kept under control with medication, in addition some have psychological problems. They require regular visits to different specialists, medical tests, transport and medication that could be expensive. As the person becomes weaker, pampers and a full-time carer is essential. Although the poor visit Government hospitals, some medicines have to be purchased from outside. But others are forced to use the private medical sector. The expenses need be funded by own savings or by the children.
Meanwhile, some other elders suffer from dementia, Alzheimer’s and Parkinson’s disease or cancer, are bed-ridden, require nasal feeding or with urinary catheters, are difficult to be looked after in their own houses, are cared for in specialist care homes and their charges could vary. But as the organisation depends on long-term caring for elders, strict instructions regarding extent of care would be necessary.
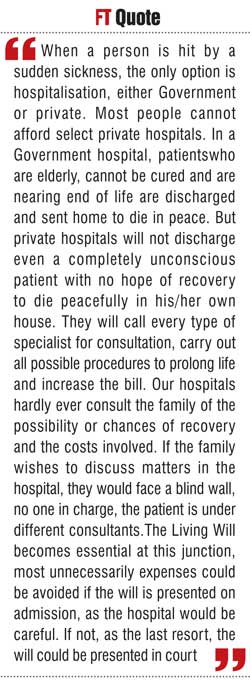
But when a person is hit by a sudden sickness, the only option is hospitalisation, either Government or private. Most people cannot afford select private hospitals. In a Government hospital, patients who are elderly, cannot be cured and are nearing end of life are discharged and sent home to die in peace.
But private hospitals will not discharge even a completely unconscious patient with no hope of recovery to die peacefully in his/her own house. They will call every type of specialist for consultation, carry out all possible procedures to prolong life and increase the bill. Our hospitals hardly ever consult the family of the possibility or chances of recovery and the costs involved. If the family wishes to discuss matters in the hospital, they would face a blind wall, no one in charge, the patient is under different consultants.
The Living Will becomes essential at this junction, most unnecessarily expenses could be avoided if the will is presented on admission, as the hospital would be careful. If not, as the last resort, the will could be presented in court.
Sri Lanka does not have legal provisions such as the ‘Patient Self-Determination Act’ as in USA, but it is time to enlighten the public and the Government and force them to implement a similar act.
For the young, poor road conditions without warnings, wet surfaces and reckless drivers make roads unsafe and there is always the risk of accident. A Living Will, irrespective of whether one is young or elderly in their final hours of living, will make decisions easier and less painful for loved ones.